Addressing the HIV and Tuberculosis Crisis in Zimbabwe
Zimbabwe is facing a critical public health challenge, marked by the concurrent epidemics of HIV and tuberculosis (TB). This dual health crisis significantly endangers both the healthcare infrastructure and the overall health of its population. According to data from the Centers for Disease Control and Prevention (CDC), the intersection of these two infectious diseases complicates efforts for healthcare professionals and public health authorities. With one of the highest global rates of HIV, individuals are at an elevated risk for TB, underscoring the need for integrated healthcare strategies that emphasize holistic patient management. This article delves into Zimbabwe’s current situation regarding HIV and TB, offering recent statistics, persistent challenges, and vital interventions required to combat these interconnected diseases through CDC initiatives alongside local healthcare responses. It becomes clear that targeted actions are essential to improve health outcomes while alleviating the impact of these epidemics on Zimbabwean society.
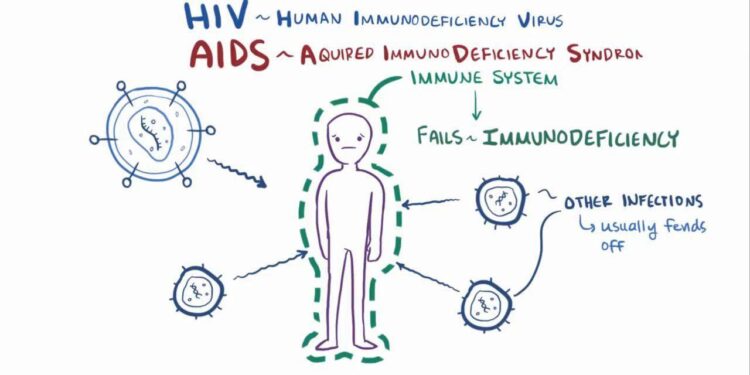
Understanding the Link Between HIV and TB in Zimbabwe
The interplay between HIV infection and tuberculosis (TB) presents a significant public health obstacle within Zimbabwe. The high prevalence rate of HIV among its citizens creates conditions favorable for TB transmission since HIV severely weakens immune defenses, heightening vulnerability to infections. Studies reveal that individuals living with HIV are roughly 20 to 37 times more likely to develop active TB compared to those who do not have this virus. This concerning relationship is exacerbated by their shared modes of transmission, further straining Zimbabwe’s already burdened healthcare system.
In light of this dual epidemic, various integrated intervention strategies have been implemented across Zimbabwe aimed at enhancing diagnosis capabilities, treatment accessibility, and prevention measures for both diseases. Key initiatives include:
- Fostering collaboration among service providers addressing both conditions.
- Increasing access to screening services for early identification of both illnesses.
- Educating communities about risks associated with each disease along with effective preventive strategies.
This comprehensive approach is crucial in addressing rising cases of TB among those living with HIV while working towards reducing morbidity rates throughout communities. Below is a summary table showcasing key statistics related to this intertwined epidemic:
| Year | % Prevalence Rate for HIV | Tuberculosis Incidence (per 100k) | ||||
|---|---|---|---|---|---|---|
| 2019 | 11.9% | 400 | ||||
| 2020 | 12.5% | 525 | ||||
| 2021 | 13.1% | 480
Current Trends & Healthcare ObstaclesThe ongoing relationship between tuberculosis (TB) and human immunodeficiency virus (HIV) continues presenting considerable challenges within Zimbabwe’s healthcare landscape-compounded by socioeconomic factors as well as limitations within medical facilities . Currently estimated at around13% , nearly one-seventh of adults live either actively infected or previously diagnosed involving AIDS/HIV; concurrently facing disproportionately high incidences directly linked back towards co-infection scenarios where patients also contract tuberculosis-demonstrating how individuals infected by either pathogen face up-to30 times greater likelihoods of developing secondary infections like active forms associated specifically towards mycobacterium species responsible behind causing pulmonary complications leading into full-blown clinical presentations requiring immediate attention from trained professionals capable managing such complexities effectively! A multifaceted strategy has emerged focusing on critical areas necessary combatting intertwined epidemics:
|